
Diagnosis: Ultrasound (transabdominal or endoscopic). Black pigment stones ( 1 cm are carcinomas 
Rule of the 6 Fs : F at, F emale, F ertile, F orty, F air-skinned, F amily history. Increased progesterone levels cause smooth muscle relaxation, decreased and impaired gallbladder contraction, and subsequent bile stasis and formation of gallstones.
Pathophysiology: abnormal hepatic cholesterol metabolism → ↑ cholesterol concentration in bile and ↓ bile salts and lecithin → hypersaturated bile → precipitation of cholesterol and calcium carbonate → cholesterol stones or mixed stonesĭuring pregnancy, increased estrogen levels cause increased secretion of lithogenic bile (rich in cholesterol ), resulting in the formation of cholesterol gallstones. Malabsorption (e.g., Crohn disease, ileal resection, cystic fibrosis ). Drugs: fibrates (inhibition of cholesterol 7-α hydroxylase), estrogen therapy, oral contraceptives. European, Native American, or Hispanic ancestry. Increased progesterone levels cause smooth muscle relaxation, decreased gallbladder contraction, and subsequent bile stasis with formation of gallstones. Increased estrogen levels cause increased secretion of bile rich in cholesterol, (lithogenic bile), which can result in the formation of cholesterol gallstones. Especially during reproductive years due to increased levels of estrogen and progesterone. Obesity, insulin resistance, dyslipidemia. Impaired gallbladder emptying (e.g., due to bowel rest, prolonged total parenteral nutrition, pregnancy ) → biliary sludge → bile stasis ( cholestasis)Ĭholesterol stones (up to 95% of all stones). Biliary stasis is a key component in gallstone formation. Imbalance in bile salts, lecithin (stabilizer), cholesterol, calcium carbonate, and bilirubin. 10–20% of the adult population in developed countriesĮpidemiological data refers to the US, unless otherwise specified. See “ Acute management checklist for acute cholangitis.”. Interval cholecystectomy if gallstones are present or concurrent cholecystitis. See “ Acute management checklist for acute cholecystitis.”. Cholecystectomy (timing depends on severity). See “ Acute management checklist for choledocholithiasis.”. Elective cholecystectomy to prevent recurrence. See “ Acute management checklist for biliary colic.”. Asymptomatic cholelithiasis only if at increased risk of gallbladder cancer. US: biliary dilation, and/or evidence of obstruction (e.g., cholelithiasis), pericholecystic inflammation. HIDA scan: nonvisualization of gallbladder > 4 hours after radioactive tracer administration. US: gallbladder wall thickening and/or edema (double wall sign).  MRCP or ERCP: filling defect in the contrast-enhanced duct. US: dilated common bile duct, intrahepatic biliary dilatation. US: gallstones with posterior acoustic shadow.
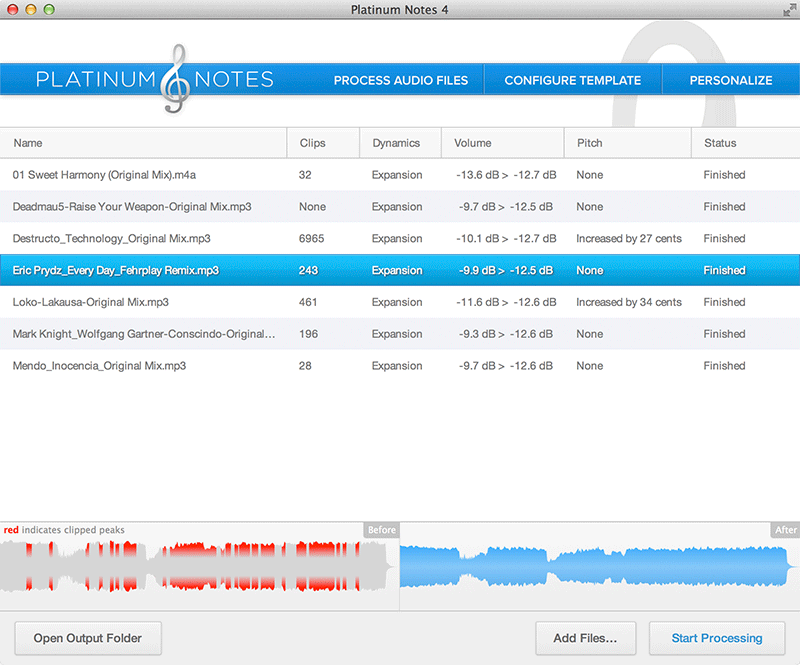
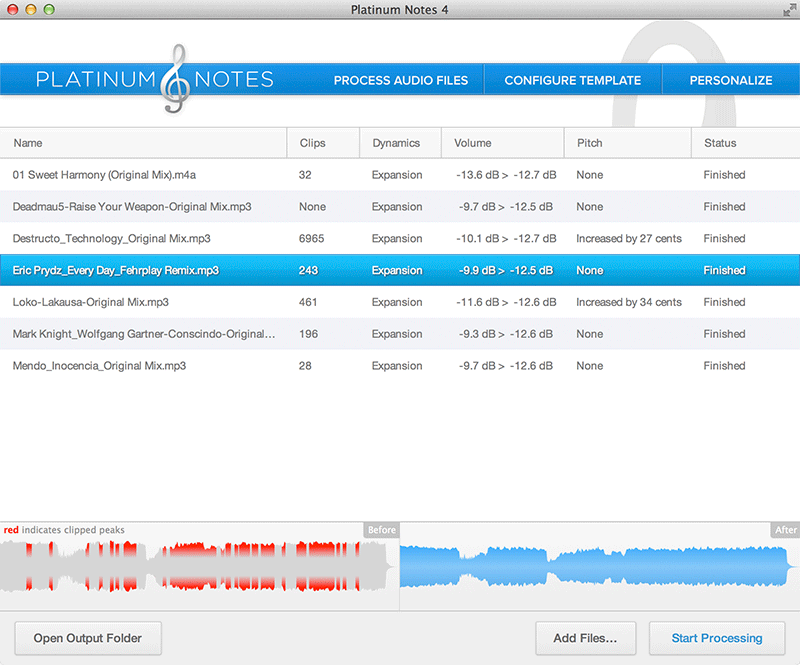
MRCP or ERCP: filling defect in the contrast-enhanced duct. US: dilated common bile duct, intrahepatic biliary dilatation. US: gallstones with posterior acoustic shadow. Platinum notes alternative plus#
Reynold pentad: Charcot cholangitis triad PLUS hypotension and mental status changes. Charcot triad: RUQ pain, fever, jaundice. Symptomatic ( biliary colic): RUQ pain 6 h. Choledocholithiasis (most common) → obstruction and stasis within the biliary tract → subsequent bacterial infection. 
Cholelithiasis (most common) or biliary sludge → inflammation of gallbladder wall. Cholelithiasis → migration of gallstones into the common bile duct. Bile cholesterol oversaturation, bile stasis, impaired bile acid circulation → precipitation of gallstones in the gallbladder. Bacterial infection of the biliary tract. Presence of gallstones in the common bile duct. Presence of gallstones in the gallbladder.






 0 kommentar(er)
0 kommentar(er)
